Understanding Sacroiliac Joint Dysfunction: What You Need to Know
Sacroiliac joint dysfunction is a common yet often overlooked cause of lower-back and pelvic pain. The good news? It doesn’t always require surgery. With the right care, targeted rehab, postural correction, and learning what to watch for. You can stabilise your pelvis, reduce pain, and move with confidence again.
Here’s a guide to what the SI joint is and what happens when it becomes dysfunctional, how it’s diagnosed, what treatment options exist (both non-surgical and surgical), and how you can protect your lower back long term.
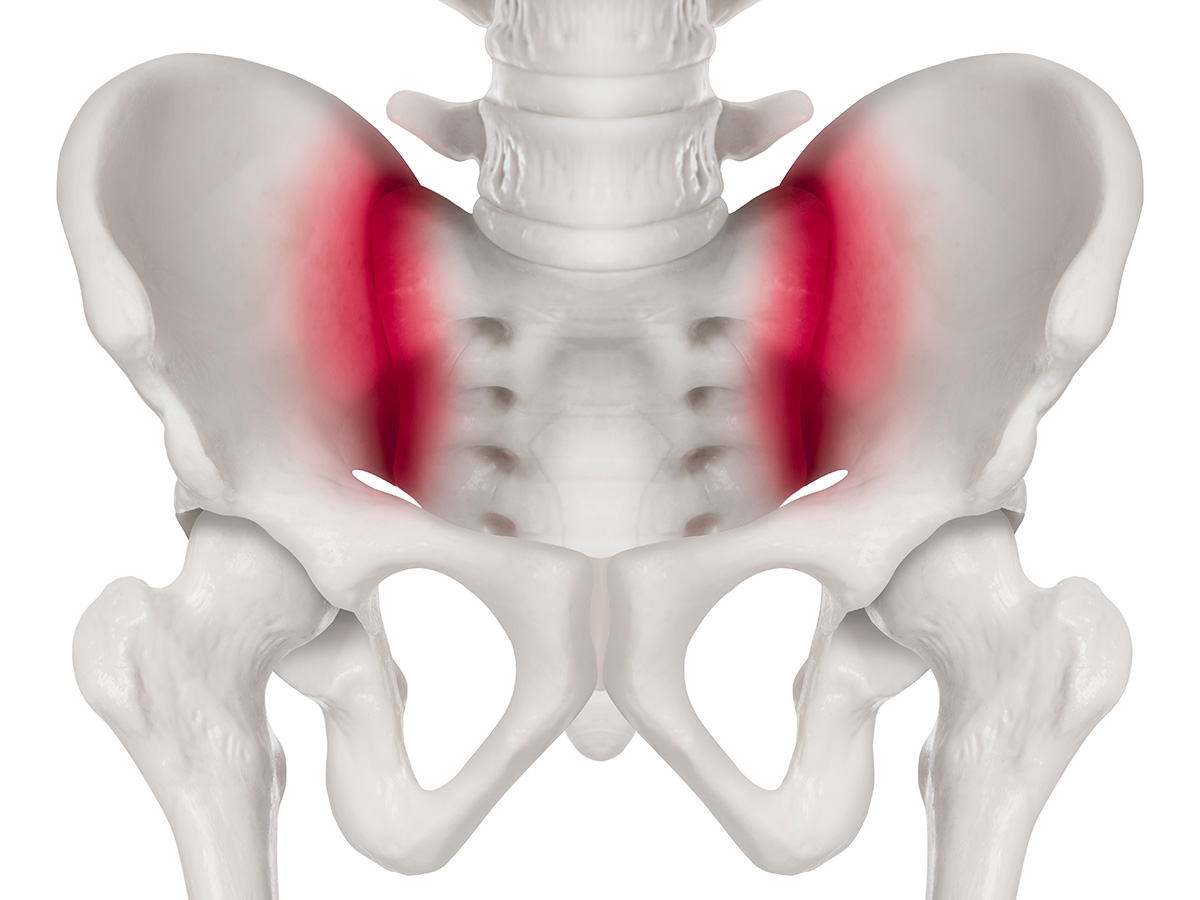
Why the Sacroiliac Joint Matters
The sacroiliac joint connects the base of your spine (the sacrum) with your pelvis (the iliac bones). You have one on each side, forming the link between your upper body and your legs.
It helps by:
- Absorbing shock and distributing load between your spine, pelvis, and legs
- Providing stability while allowing small, controlled movements for bending, walking, and twisting
- Protecting surrounding structures, such as the lumbar spine and hips, from excess strain
When the SI joint becomes too stiff or too mobile, it can place extra stress on nearby tissues, leading to pain, imbalance, and movement issues.
How SI Joint Dysfunction Happens
SI joint dysfunction can occur in several ways:
- Too much movement (hypermobility/instability): The ligaments supporting the joint may become lax due to pregnancy, trauma, or previous surgery, leading to instability and discomfort in the lower back, hip, or groin.
- Too little movement (hypomobility/fixation): When the joint becomes overly tight or “locked,” it can restrict normal motion and cause local pain or stiffness.
- Degenerative or inflammatory changes: Conditions such as osteoarthritis, ankylosing spondylitis, or general wear and tear can cause irritation to the joint.
- Repetitive stress or imbalance: Standing or sitting for long periods, uneven leg length, or previous spinal fusion can overload one side of the pelvis and irritate the joint.
Recognising the Symptoms
Common signs of SI joint dysfunction include:
- Pain on one side of the lower back, buttock, or hip
- Pain that may radiate into the groin or down the leg (similar to sciatica)
- Stiffness or soreness after sitting or standing for long periods
- Discomfort when changing positions e.g., standing up from a chair or climbing stairs
- A sensation of instability or “giving way” in the pelvis or lower back
Diagnosing SI Joint Dysfunction
Diagnosis involves a combination of:
- Clinical examination: Your practitioner will assess movement patterns, tenderness, and perform specific SI joint provocation tests.
- Imaging or diagnostic injections: An MRI or X-ray may help rule out other causes. Sometimes, an anaesthetic injection into the SI joint helps confirm if it’s the pain source.
- Exclusion of other conditions: SI joint pain can mimic disc or hip problems; a thorough assessment ensures an accurate diagnosis.
Treatment Options
Conservative (Non-Surgical)
Most SI joint issues can be effectively managed without surgery through:
- Rest and modification of activities: avoid movements or positions that worsen pain
- Physical therapy / Chiropractic care: tailored exercises and manual therapy to restore alignment, improve mobility, and strengthen core and hip muscles
- Supportive bracing: SI belts can help stabilise the joint during flare-ups
- Pain management strategies: anti-inflammatory medication, ice/heat therapy, or other therapeutic modalities to reduce discomfort
- Postural and ergonomic advice: learning to move and lift properly to protect the joint
Surgical
If conservative care doesn’t provide relief, and imaging confirms the SI joint as the source of pain, surgery may be considered:
- SI joint fusion — a minimally invasive procedure that stabilises the joint by joining the sacrum and ilium using specialised implants
- Other procedures — such as steroid injections or radiofrequency ablation may help reduce inflammation or pain before fusion is considered
Recovery & Rehabilitation
Recovery time varies depending on the cause and treatment. Rehabilitation focuses on:
- Restoring comfortable, pain-free movement
- Strengthening surrounding muscles (core, glutes, hips, hamstrings) for stability
- Improving posture and movement control
- Addressing leg length discrepancies or other biomechanical issues to prevent recurrence
With consistent care, many people experience significant improvement within a few weeks to months.
Protecting Your Pelvis & Lower Back Long-Term
To keep your SI joints healthy:
- Warm up before exercise or physical activity
- Maintain strong glutes, hips, and core muscles
- Avoid prolonged sitting or standing in one position
- Use correct lifting technique: bend at the knees, avoid twisting
- Keep good posture at work and home
- Seek early advice if pain returns or you notice asymmetry in movement
We’re Here to Help
At Chiro & Sports Med, we understand how frustrating lower-back and pelvic pain can be; especially when it holds you back from doing the things you love. Whether you’re managing sacroiliac joint dysfunction, recovering from an injury, or need a personalised rehab plan, our experienced team is here to support you every step of the way.
📞 Call us at (02) 9817 2005 or Book Online to schedule an appointment and get expert help today.